Eye Diseases
Questions:
What Is Allergic Eye Disease?
What it is Blepharitis?
What Is A Chalazion?
What Is A Corneal Abrasion?
What Is Diabetic Retinopathy?
What Is Dry Eye?
What Is Ectropion?
What Is Entropion?
What Are Flashers And Floaters?
What Is Glaucoma?
What Is Macular Degeneration?
What Is Migraine Syndrome?
What Is Ptosis?
What Is A Retinal Detachment?
Allergic Eye Disease
What Is Allergic Eye Disease?
Allergic eye disease is often known as allergic conjunctivitis, and is an inflammation of the conjunctiva caused by an allergic reaction. The two most common forms of allergic eye disease include seasonal allergic conjunctivitis and perennial allergic conjunctivitis. Seasonal allergic conjunctivitis is often associated with the effects of hay fever. Perennial allergic conjunctitivitis often occurs on a year round basis and its prominence is attributed mainly to permanent contact with the allergen. In perennial allergic conjunctivitis the most common allergen is house dust or pet dander.
Are There Other Forms Of Allergic Eye Disease?
There are other forms of allergic eye disease and are often the less common forms of allergic eye disease. Some of these less common forms include:
Atopic Keratoconjunctivitis - Atopic keratoconjunctivitis is a chronic, bilateral inflammation of the eyelids and conjunctiva and is often associated with atopic eczema
Vernal Keratoconjunctivitis - Vernal keratoconjunctivitis is a rare but chronic bilateral disease occurring mostly in children who have a history of atopy
Giant Papillary Conjunctivitis - Giant papillary conjunctivitis is an inflammatory disorder of the superior tarsal conjunctiva. Giant papillary conjunctivitis often occurs in the presence of a foreign body and is often the result of contact lens use.
What Are the Symptoms of Allergic Eye Disease?
The more common symptoms of allergic eye disease include:
• Red eyes or eyelids
• Increased tearing
• Itchy eyes
• Blurred vision
• Swelling of the eyelid or eyelids
Please contact our offices and schedule an appointment if you are experiencing any of these symptoms.
How Is Allergic Eye Disease Treated?
Allergic eye disease may disappear completely when the allergy is treated with antihistamines or when the allergen has been removed. For treatment of allergic eye disease, our doctor's may advise one or more of the following:
Topical Ocular Decongestants - This form of medicine reduces redness of the eye by constricting small blood vessels. Topical ocular decongestants are very affective, but are not recommended for long-term use. It is possible that overuse of this medicine can actually worsen symptoms if used for more than a few days.
Topical Ocular Antihistamines - The use of this medicine reduces eye redness, itching and swelling by blocking the actions of histamine. Histamine is the chemical that causes these symptoms of allergic eye disease. This form of medication is available over-the-counter and by prescription.
Topical Ocular Steroids - If other forms of medication do not seem to be helping you, please contact our offices and inform our staff so we may provided you with proper treatment. Our doctor's may prescribe you with steroid eye drops to relieve the symptoms of allergic eye disease. This medication must be used with the supervision of our doctor's because the use of topical ocular steroids can cause an increase in your intraocular pressure. An increase in your intraocular pressure can cause damage to your vision. Our doctor's will also look for any signs of a viral eye infection like ocular herpes, before prescribing the use of topical ocular steroids. It is also possible that the use of topical ocular steroids will increase your chances of developing cataracts.
Cromolyn - This medication is recommended for use before symptoms of allergic eye disease occur, and works by stopping specialized cells from releasing histamine.
Immunotherapy - Allergy shots provided by your doctor can be effective in stopping the effects of allergic eye disease.
What Else Can I Do To Help My Allergic Eye Disease?
To relieve some of the symptoms of allergic eye disease, our doctor's recommend the use of following:
• If you are a contact lens wearer, we suggest you remove them and wear your glasses for a while
• The use of cold compresses placed over your eyes
• The use of artificial tears may help relieve some of the symptoms of allergic eye disease. Artificial tears are an eye drop that can help relieve the itching and burning caused by allergic eye disease. We do not recommend that you use the same bottle of drops in the other eye if it is not affected by allergic eye disease. Using the same bottle of eye drops in the other, unaffected eye may cause that eye to become affected.
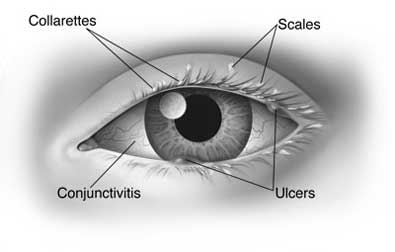
What Causes Blepharitis?
Everyone has bacteria on the surface of their skin; however some people have bacteria that thrives in the skin at the base of the eyelashes. Large amounts of bacteria around the eyelashes can cause dandruff-like scales and particles to form along the lashes and eyelid margins. Blepharitis is also associated with meiobomitis. Meiobomitis is a dysfunction and inflammation of the nearby oil glands of the eyelids. These glands are called the meiobomian glands.
How Is Blepharitis Treated?
Blepharitis is often a chronic condition, but can be controlled with treatment. The following treatments can help control blepharitis:
• Warm Compresses
• Eyelid Scrubs
• Antibiotic Ointment
• Good Hygiene
• Omega 3-6-9 Fish Oil Capsules
If you have any questions about these treatments or questions about this condition please feel free to contact our offices.
Chalazion
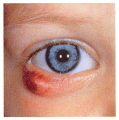
What Is A Chalazion?
The term chalazion is Greek for "small lump." Chalazion refers to a swelling in the eyelid caused by inflammation of one of the small oil producing glands located in the upper and lower eyelids. These glands are known as the meiobomian glands. Often, a chalazion is confused with a stye, which also appears as a lump in the eyelid. Unlike a chalazion, a stye is an infection of a lash follicle that forms a sore, red lump near the edge of the eyelid.
A chalazion is an inflammatory reaction to trapped oil secretions. A chalazion is not caused by bacteria, although it can become infected with bacteria. Unlike stye's, chalazion's tend to form farther from the edge of the eyelid, and tend to "point" towards the inside of the eyelid. It is not uncommon for a chalazion to cause the entire eyelid to swell suddenly, but usually there is a definite tender point.
How Is A Chalazion Treated?
When a chalazion is small and without symptoms, it may disappear on its own. When a chalazion is large, it may cause blurred vision. A chalazion is treated with any or a combination of the following methods:
• Warm Compresses
• Steroid Injections
• Surgical Incision or Excision
Chalazion's usually respond well to treatment, although some people are prone to recurrences. If a chalazion recurs in the same place, a biopsy of the chalazion may be necessary.
Corneal Abrasion
What Is The Cornea?
The cornea is the clear front window of the eye, and covers the colored portion of the eye. The cornea is composed of five layers, and the outermost layer of the cornea is called the corneal epithelium.
What Is A Corneal Abrasion?
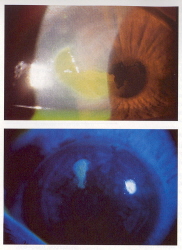
A corneal abrasion refers to a scratch or injury to the corneal epithelium. These abrasions are quite common and are painful. They result from contact lenses, tree limbs, bushes, or vigorous rubbing of the eye. Corneal disease has been understood to be a contributing factor also.
How Is A Corneal Abrasion Treated?
Copious lubrication is important for comfort and to help promote healing. An antibiotic may be prescribes to prevent infection. Anesthetic drops can relieve pain and facilitate examination but may keep the eye from healing properly if used repeatedly. Occasionally, long after an abrasion has healed it may recur suddenly. Recurrent corneal abrasions often require the use of ointments at bedtime. In some cases a soft or bandage-type contact lens is used to facilitate healing.
What Problems May I Have?
If bacteria gets into the tissues under the protective corneal epithelium, infection or a corneal ulcer can occur. These can be very serious and cause vision loss if untreated. In most cases corneal abrasions will heal completely, but it is necessary to see our doctors to prevent any serious visual complications.
How Long Will It Take To Heal?
A corneal abrasion will usually heal within a week. During the healing process it is very important not to rub the affected eye. The new epithelium cells are fragile and easily be rubbed off. When the new epithelium cells are removed, the pain returns.
Diabetic Retinopathy


How Does Diabetes Affected The Eye?
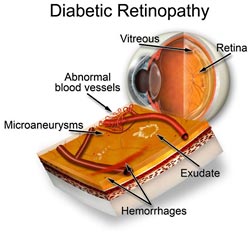
If you have been diagnosed with diabetes mellitus, your body does not use and store sugar properly. High blood-sugar levels may damage the blood vessels in the retina. This damage to the retina is known as diabetic retinopathy.
What Are The Types Of Diabetic Retinopathy?
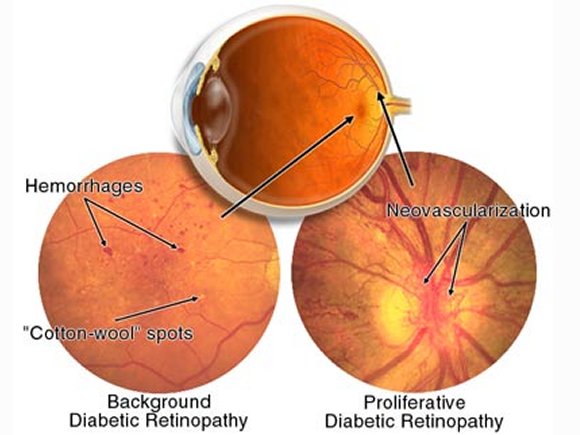
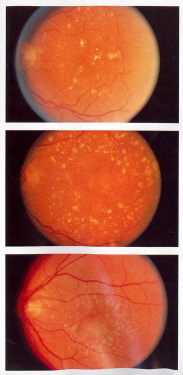
Diabetic retinopathy has been classified as two different types. Non-proliferative diabetic retinopathy, also known as NPDR, and proliferative diabetic retinopathy, also known as PDR.
Non-Proliferative Diabetic Retinopathy - NPDR has also become known as "background retinopathy," and is an early stage of diabetic retinopathy. During this stage, tiny blood vessels within the retina leak blood or fluid. The leaking fluid causes the retina to form deposits known as exudates, or swell. Many diabetics have a mild case of NPDR and their vision is usually left unaffected. However, when the vision becomes affected, it is usually the result of macular edema and/or macular ischemia.
Macular Edema - Macular edema is swelling, or thickening of the macula. The swelling is mainly caused by leaking fluid from retinal blood vessels. This is the most common cause of vision loss among diabetics. Vision loss can be mild to severe, but even in the worst cases, peripheral vision continues to function.
Macular Ischemia - Macular ischemia occurs when small blood vessels called capillaries close. Vision becomes blurry because the macula is no longer receiving sufficient blood supply for it to function properly.
Proliferative Diabetic Retinopathy - PDR is present when abnormal new vessels (neovascularization) begin forming on the surface of the retina or optic nerve. PDR is mainly caused by widespread closure of retinal blood vessels which prevents and restricts adequate blood flow. The retina responds to this by creating new blood vessels in an attempt to supply blood to the area where the original vessels have closed.
These new, abnormal blood vessels do not re-supply the retina with normal blood flow. These new blood vessels are often accompanied by scar tissue that may cause wrinkling or detachment of the retina. PDR may cause more severe vision loss than NPDR because it can affect both central and peripheral vision.
PDR causes vision loss in the following ways:
Vitreous Hemorrhage - The fragile new vessels may bleed into the vitreous of the eye. If the vitreous hemorrhage is small only a few new dark floaters may be noticed. If the vitreous hemorrhage is large it may block out all vision in that eye. It may take the eye days, months or even years to resorb the blood, dependent upon how much blood is present. If the blood in the vitreous is not adequately cleared by the eye within a reasonable time span, vitrectomy surgery may be needed. This is performed by a retina specialist. A vitreous hemorrhage alone cannot cause vision loss. However, when the blood clears, visual acuity may return to its former level unless the macula is damaged.
Traction Retinal Detachment - When PDR is present, scar tissue associated with neovascularization can shrink, causing the retina to wrinkle and be pulled from its original position. Macular wrinkling can cause visual distortion, and more severe vision loss can occur if the macula or large areas of the retina are detached.
Neovascular Glaucoma - Occasionally, extensive retinal vessel closure will cause new, abnormal blood vessels to grow on the iris and block the normal flow of fluid out of the eye. Due to the abnormal flow, pressure in the eye builds up resulting in neovascular glaucoma. Neovascular glaucoma is a severe eye disease that causes damage to the optic nerve.
How Is Diabetic Retinopathy Diagnosed?
Having a comprehensive eye examination is the only real way to find changes inside your eye. It is often possible to diagnose and treat serious retinopathy before you are aware of any problems with your vision. During the eye examination our doctor will dilate you and look inside your eye using an ophthalmoscope. It may be necessary to take color photographs of the retina or have a special test called fluorescein angiography to find out if you need treatment. With the fluorescein angiography test, dye is injected into your arm and photos of the eye are taken to detect if there is fluid leaking.
-
How Is Diabetic Retinopathy Treated?
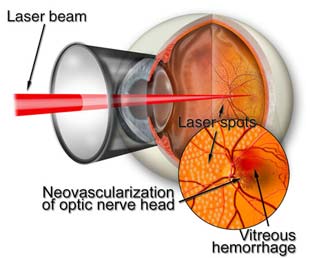
The number one recommended treatment is to prevent the development of diabetic retinopathy as much as possible. This can be done by strict control of your blood sugar which will significantly reduce the long-term risk of vision loss fro diabetic retinopathy. Below are a few ways in which diabetic retinopathy can be treated:Laser surgery: Often recommended for people with macular edema, proliferative diabetic retinopathy and neovascular glaucoma.
Macular Edema: For macular edema, the laser is focused on the damaged retina near the macular to decrease the fluid leakage. The main goal of treatment is to prevent further loss of vision. It is uncommon for people who have blurred vision from macular edema to recover normal vision, although some may experience partial vision gains. Some people may see the laser spots near the center of their vision following treatment. These spots usually fade with time, but may not disappear completely. As the diabetes progresses it is often necessary to treat new areas of edema.
Proliferative Diabetic Retinopathy: For PDR, the laser is focused on all parts of the retina except the macula. This treatment is called panretinal photocoagulation which causes abnormal new vessels to shrink and often prevents them from growing in the future. This treatment also reduces the chance of vitreous bleeding or retinal distortion to occur. Over time, it may be necessary for multiple laser treatments. Laser surgery does not cure diabetic retinopathy and does not always prevent further loss of vision.
Vitrectomy: In advanced cases of PDR it may be necessary for the patient to have a vitrectomy. The vitrectomy microsurgical procedure is performed in an operating room and involves removing the blood filled vitreous of the eye and replacing it with a clear solution. Vitrectomy often prevents further bleeding by removing the abnormal vessel that caused the bleeding. If the retina is detached, it can be repaired during the vitrectomy surgery procedure. Surgery is often done early because macular distortion or traction retinal detachment will cause permanent visual loss. The longer the macular is distorted or out of place, the more serious the vision loss will become.
Is Vision Loss Preventable?
Largely due to today's improved methods of diagnosis and treatment only a small percentage of individuals who have diabetes and develop retinopathy have serious visual problems. The best prevention of vision loss is early detection of diabetic retinopathy. You can significantly lower your risk of vision loss by maintaining strict control of your blood sugar, seeing our doctors regularly, and keeping your appointments with your primary doctor and our offices.
Dry Eye Disease
What Is Dry Eye?
Some people do not produce enough tears to keep the eye comfortable and these individuals have what is known as Dry Eye. There are two methods of natural production of tears. One method is responsible for normal eye lubrication in which tears are produced at a slow steady rate. Another method produces a large amount of tears in a short period in response to eye irritation or emotions (crying).What Are The Symptoms Of Dry Eye?
The common symptoms most individuals who have dry eye experience are:• Stinging or burning eyes
• Scratchy eyes
• Stringy mucus in or around the eyes
• Eye irritation from smoke or wind
• Excessive tearing
• Difficulty wearing contact lensesIt may be hard to believe, and it may sound illogical, but excessive tearing from dry eye is possible. If the tears responsible for normal lubrication do not keep the eye wet enough, the eye becomes irritated. When the eye becomes irritated, the lacrimal gland produces a large volume of tears which overwhelms the tear drainage system. The excessive amount of tears then overflows from your eye.
What Is The Tear Film?
The tear film is a film of tears spread over the eye by a blink, and helps make the surface of the eye smooth and clear. Without the tear film, good vision would be practically impossible. The tear film is comprised of three layers including:• An oily layer
• A watery layer
• A layer of mucusThe oily layer, which is produced by the meiobomian glands, forms the outermost surface of the tear film. The oily layer's main purpose is to smooth the tear surface and reduce evaporation of tears. The middle watery layer makes up most of what we ordinarily think of as tears. This layer, produced by the lacrimal gland, cleans the eye and washes away any foreign particles or irritants. The inner most layer consists of mucus produced by the conjunctiva. The production of mucus allows the watery layer to spread evenly over the surface of the eye and helps the eye remain wet. Without the mucus produced by the eye, tears would not adhere to the eye.
What Causes Dry Eye?
As we age, tear production naturally decreases. Although dry eye can occur at any age, and in both men and women, women are most often affected. This is especially true for women after menopause.Dry eye can also be associated with arthritis and accompanied by a dry mouth. Individuals who have dry eyes, dry mouth and arthritis are said to have what is known as Sjorgen's syndrome. Reduced tear production causes dry eye, and there are a wide variety of common prescribed, and over-the-counter medications that can cause dry eye. Some of these include:
• Diuretics
• Betablockers
• Antihistamines
• Sleeping Pills
•"Nerve" medications
• Pain relieversThese medications are often necessary, and the dry eye condition may have to be tolerated or treated using artificial tears. Individuals with dry eye are often more prone to the negative side effects of eye medications, including artificial tears.
How Is Dry Eye Diagnosed?
Diagnosing dry eye is usually done by examining the eyes; however, sometimes tests that measure tear production may be used. The Schirmer tear test involves placing filter paper strips under the lower eye lids to measure the rate of tear production under various conditions. Another method uses a diagnostic drop, either fluorescein or rose bengal, to look for certain staining patterns.
How Is Dry Eye Treated?
Eye drops called artificial tears, which are similar to your own tears, may be used. Artificial tears lubricate the eyes and help maintain moisture. Artificial tears are available without a prescription, and there are many brands to choose from, so it may be beneficial to try several to find the right one for you.If you are sensitive to the preservatives in artificial tears, preservative-free eye drops are available. Artificial tears can be used as often as necessary, but if you have to use artificial tears more than every two hours, it may be better for you to use preservative-free brands. Artificial tears can be used once or twice daily or several times an hour.
Conserving your eyes' own tears is another approach to keeping your eyes moist. Tears drain from the eye through a small channel into the nose, and it may be necessary to either temporarily or permanently close the channel. The closing of the channel allows conservation of your own tears and makes artificial tears last longer.
Tears, like other liquids, will evaporate. There are steps you can take to minimize evaporation. In the winter months when indoor heat is on, a humidifier or pan of water placed on or near the heat source will add moisture to the air. Anything that may cause dryness should be avoided by an individual with dry eye. These include an overly warm room, hair dryers, and smoking. Some people with dry eye complain of "scratchy eyes" when they wake up. This can be treated by using an artificial tear ointment at bedtime.
Are There Other Methods Of Treatment?
For some patient's, punctal plugs or lacrimal plugs may be inserted painlessly in our offices, and are normally not felt once inserted. Punctal plugs or lacrimal plugs are temporary or permanent silicone plugs inserted in the lacrimal (tear) ducts of the eye to keep the natural tears your eye produces from draining away quickly.There is also a new type of punctal plug that is made of acrylic that can also be used. The acrylic punctal plugs are a small rod that becomes a soft gel after being inserted and after becoming exposed to your body heat. These punctal plugs are designed to form to the size of any punctum canal. The overall advantages of this type of punctal plug are that one size fits all so no measurements are necessary, and there is also nothing to protrude from the tear duct that could potentially cause irritation.
Ectropion

What Is Ectropion?
Ectropion is a sagging of the lower eyelid which allows the eye to be exposed causing dryness of the eye. Ectropion is caused by a lack of tone of the muscle that holds the lid against the eye. Excessive tearing is a common sign of ectropion, and wiping the tears from the eye only causes the lid to sag more. Ectropion is more common in people over the age of 60.What Are The Signs & Symptoms Of Ectropion?
Ectropion has some distinctive signs and symptoms, but the more common ones are located below. Ectropion should not be confused with dry eye syndrome even with both having similar signs and symptoms.• Irritation of the eye
• Burning or stinging
• Having a gritty, sandy feeling
• Excessive tearing
• Red, irritated eyelid or eyelidsHow Is Ectropion Diagnosed?
In patients who have or are believed to have ectropion, the best way to diagnose the condition is through a routine eye examination with our office.How Is Ectropion Treated?
With ectropion comes eye irritation with can be temporarily relieved artificial tears and ointments that lubricate the eye. To treat ectropion, surgery is often needed to tighten the lid.
Entropion
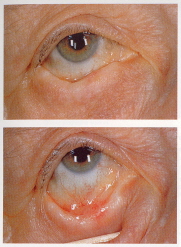
What Is Entropion?
Entropion is when an eyelid is turned inward, and is a problem that usually affects the lower eyelid. Entropion is usually caused by a muscle spasm, but can also be caused by scarring from trauma or even inflammation from certain diseases the affect the eyelids. When the eyelid is turned inward, the lashes rub against the eye causing eye irritation, foreign body sensation, tearing and redness.What Are The Signs & Symptoms Of Entropion?
Entropion has some distinctive signs and symptoms, but the more common ones are located below. Entropion should not be confused with dry eye syndrome even with both having similar signs and symptoms.• Excessive tearing
• Burning or stinging
• Irritation
• Sandy, gritty feeling
• Red eyeHow Is Entropion Diagnosed?
Entropion can easily be detected during a routine eye examination with our office. Our doctor's use a slit lamp microscope to examine the effects that the in-turned eyelashes have caused on the surface of the eye. From here our doctor's will advise you on the best method of treatment.
How Is Entropion Treated?
For treatment of entropion, the most effective method is surgery. If you would prefer not to have surgery, our doctor's can advise you of other alternative methods of treatment. However, to permanently treat the effects of entropion, surgery is often the only method of treatment. For some people artificial tears are helpful to ease the irritation caused by the lashes rubbing against the eye.
Flashers And Floaters
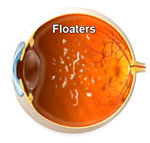
What Are Floaters?
Floaters are generally small specks or clouds you may see in your field of vision. They are usually most noticeable when you look at a plain background, like a blank wall or blue sky. Floaters are found in the vitreous of the eye and are composed of tiny clumps of gel or cells. When floaters are seen, they appear to be in front of the eye, but are actually floating inside the eye. Floaters can have different shapes, but the most common are little dots, circles, lines, clouds and cobwebs.What Causes Floaters?
The vitreous gel of the eye may start to thicken or shrink, which forms clumps or strands in the eye in middle aged people. The vitreous gel begins to pull away from the back wall of the eye causing what is known as a posterior vitreous detachment. Posterior vitreous detachment is a common cause of floater, but is more common in people who:• Have nearsightedness
• Have had cataract surgery
• Have had YAG laser eye surgery
• Have had inflammation inside the eyeAre Floaters Serious?
If the shrinking vitreous gel pulls away from the wall of the eye, the retina can tear. This may cause a small amount of bleeding in the eye that may appear as floaters. A torn retina is always a serious problem mainly because it can lead to retinal detachment.Is There A Cure For Floaters?
If floaters appear suddenly, it is highly recommended you contact either of our offices to schedule an appointment to see if your retina is torn. Floaters can become quite bothersome and can get in the way of your vision, especially during reading. When floaters are bothering you, you can try moving your eyes up and down to move the floaters out of the way. Some floaters may remain in your vision, however most floaters will fade over time and become less bothersome. Some patients may have floaters for several years, but it is recommended to have an eye examination immediately if you notice new floaters.What Causes Flashing Lights?
Flashing lights or lightning streaks are caused when the vitreous gel rubs or pulls on the retina. These flashing lights may appear and disappear for several weeks or months. It is more common for aging individuals to experience flashing lights. Flashing lights are associated with the loosening or movement of the vitreous gel. The gel can pull or tug on the retina. This can lead to a retinal hole, tear, or detachment. This is a serious and potentially blinding event and requires prompt evaluation and treatment. If you notice the sudden appearance of flashing lights, you should contact either of our offices to schedule an appointment.
Glaucoma

What Is Glaucoma?
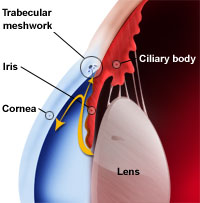
Glaucoma is a disease of the optic nerve, which is the part of the eye that carries images to the brain. The optic nerve of the eye consists of many nerve fibers, and is very fragile. If pressure inside the eye increases, damage to the optic nerve fibers may occur. If the optic nerve fibers do receive damage, blind spots will develop. Unless the optic nerve is significantly damaged, these blind spots will go undetected. If the optic nerve becomes completely damaged or destroyed, the result is complete blindness. The best prevention for glaucoma is early detection. Glaucoma is the leading cause of blindness in the United States; this is especially true for older individuals.What Causes Glaucoma?
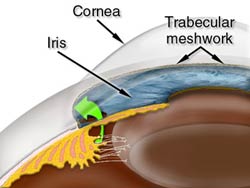
A clear liquid called the aqueous humor circulates inside the front portion of the eye. This liquid is constantly being produced by the eye while an equal amount of fluid flows out of the eye through a microscopic drainage system to maintain a constant level of pressure inside the eye. The microscopic drainage system within the eye is known as the drainage angle. The eye is a closed structure and if the drainage angle becomes blocked the excess fluid cannot flow out of the eye. The fluid flowing back into the eye will increase the pressure within the eye which will push against the optic nerve and potentially cause damage.What Are The Types Of Glaucoma?
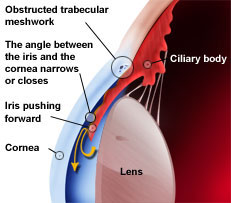
Chronic Open-Angle Glaucoma: Chronic open-angle glaucoma is the most common form of glaucoma in the United States. The risk of developing this form of glaucoma increases with age. As we age the drainage angle of the eye becomes less and less efficient. With the drainage angle becoming less efficient, the pressure within the eye will increase gradually, and possibly damage the optic nerve. It is possible for some patient's to experience a sensitivity to normal eye pressure and are at risk for optic nerve damage. Chronic open-angle glaucoma causes damage to vision so gradually and painlessly that you are not aware that your optic nerve has problems until it is already damaged.
Angle-Closure Glaucoma: Sometimes the drainage angle of the eye may become blocked. The iris of the eye may drop over top of the drainage angle and completely close it off. When this happens, eye pressure builds up suddenly and an acute angle-closure glaucoma attack occurs. Below are some of the more common symptoms of an attack:
• Vision is blurred
• Sever pain in the eye
• Headache
• Rainbow colored halo's around lights
• Nausea and vomitingHaving an acute angle-closure glaucoma attack is a serious eye emergency. If you are experiencing any of these symptoms, please call our office immediately. If this type of glaucoma is not treated promptly, blindness can occur. It is possible to experience glaucoma with both features of chronic open-angle glaucoma and acute angle-closure glaucoma. This may be referred to as either chronic angle-closure glaucoma or mixed mechanism glaucoma.
Who Is At Risk For Glaucoma?
Our doctor's take into consideration many different types of information to determine if you are at risk for developing glaucoma. Glaucoma most often occurs in adults after the age of 40, but can also occur in young adults, children and even infants. In patients who are African-American, glaucoma occurs more frequently and at an earlier age, also with a greater chance of vision loss. Our doctor's look at many different factors, but focus largely on the following:• What is the age of the patient
• Is the patient over the age of 40
• Is there a family history of glaucoma
• Does the patient have poor vision
• Is the patient of African ancestry
• Does the patient have diabetes
• Does the patient have any past eye injuriesOur doctor's look closely at these factors and will be able to determine whether you will need treatment for glaucoma, or if you should be closely monitored as a glaucoma suspect. The term glaucoma suspect refers to a patient whose risk for developing glaucoma is higher than normal. If you are a glaucoma suspect it is important that you have comprehensive eye examinations regularly to detect any early signs of damage to your optic nerve.
How Is Glaucoma Detected?
The best way to detect the early signs of glaucoma is to have comprehensive eye examinations regularly with our offices. For a glaucoma evaluation our doctor's will perform the following:
• Check your intraocular pressure
• Examine the drainage angle of the eye
• Examine the optic nerve for any damage
• Test the peripheral vision of both eyes
• Perform GDX testing of the nerve and nerve layersOur doctor's may determine during the examination that photograph's of the optic nerve are necessary. It is possible that these tests may need to be repeated on a regular basis to monitor any changes with your condition.
How Is Glaucoma Treated?
The damage caused by glaucoma is irreversible. To help prevent any further damage to your eyes, our doctor's may recommend medications, eye drops, laser surgery, or surgery in the hospital. The most affective way to prevent vision loss is to have comprehensive eye examinations on a regular basis. We suggest examinations regularly because glaucoma can progress without you knowing it has, and this can cause many unwanted problems with your vision. We also suggest examinations regularly because it may be necessary to change or make adjustments to your treatment from time to time.What Medications Are Given For Glaucoma?
Glaucoma is a disease that is usually controlled with eye drops used on a regular basis. These medications help decrease your intraocular pressure, either by improving the flow through the drainage angle or by slowing the amount of aqueous fluid produced within the eye. These medications can help preserve your vision, but some patient may experience some side effects from taking them. Please contact our offices immediately if you are experiencing any side effects from taking any of the medications we have given you. Some eye drops may cause the following side effects:• A stinging sensation
• Red eyes, or redness of the skin surrounding the eyes
• Any changes in your pulse or heartbeat
• Any changes in your energy level
• Any changes in breathing patterns
• Dry mouth
• Any changes in your sense of taste
• Headaches
• Blurred visionAll prescribed medications can have adverse side effects, and all have the potential to interact with other medications you may be taking. Therefore, it is very important that you make a list of all the medications you are taking on a regular basis and bring it to our office when you have an appointment.
How Does Laser Surgery Treat Glaucoma?
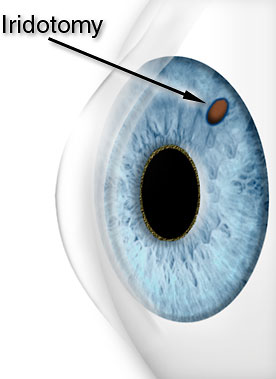
Depending on the type of glaucoma the patient has will determine the best possible laser surgery treatment. For open-angle glaucoma a treatment known as Trabeculoplasty is used to modify the drainage angle to help control eye pressure. For angle-closure glaucoma a method known as Iridotomy is used to create a hole in the iris which improves the flow of aqueous fluid inside the eye to the drainage angle.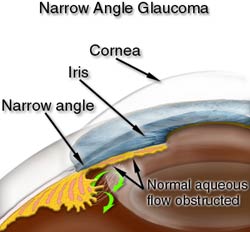
What Other Types Of Surgery Are There?
Sometimes to treat glaucoma surgery in an operating room at the hospital is needed. Our surgeon would use fine, microsurgical instruments to create a new drainage channel for the aqueous fluid to leave the eye. As with laser surgery, this type of surgery is usually done on an outpatient basis. As with all surgical procedures, there are risks. With today's advancements in medicine, serious complications with having glaucoma surgery are very uncommon, but can occur. Having this type of glaucoma surgery is recommended to prevent any further damage to the optic nerve.
Macular Degeneration And Macular Diseases
What Is Macular Degeneration?
Macular degeneration is deterioration or breakdown of the macula. The macula is a small area in the retina at the back of the eye that allows you to see fine detail clearly and allows you to read and drive. When the macula does not function properly your central vision can be affected. When your central vision is affected, you may experience blurriness, dark areas, or distortion of your vision. Macular degeneration affects your ability to see near and far, and can make some activities difficult or impossible. Macular degeneration reduces the vision in the central part of the retina, but does not affect the side or peripheral vision. Macular degeneration alone does not cause total blindness, and in many cases the impact macular degeneration has on your vision is very minimal.What Causes Macular Degeneration?
Many older individuals develop macular degeneration as part of the body's natural aging process. The most common macular problem is age-related macular degeneration, although there are other types of macular degeneration. It is not known exactly why age-related macular degeneration develops, and no uniform treatment has been effective. In individuals over the age of 65, macular degeneration has become the leading cause of severe vision loss. The most common types of age-related macular degeneration are "dry" and "wet", also known as atrophic and exudative."Dry" Atrophic Macular Degeneration: Most people who have macular degeneration have the "dry" form. "Dry" macular degeneration is caused by the aging and thinning of the tissues of the macula, and vision loss is usually gradual.
"Wet" Exudative Macular Degeneration: About 10% of all macular degeneration cases area attributed as the "wet" form. The "wet" form of macular degeneration happens when abnormal blood vessels form under the retina at the back of the eye. These abnormal blood vessels tend to leak fluid or blood which causes blurred central vision, and as a result, vision loss may be rapid or severe.
What Are The Symptoms Of Macular Degeneration?
Although there are some definite signs of macular degeneration, the symptoms can be different for different people. Macular degeneration can sometimes be hardly noticeable in its early stages, and sometimes only one eye may lose vision while the other eye remains fine for years. When macular degeneration affects both eyes, the loss of the central vision can be noticed more quickly. Some common ways vision loss is detected:• Words on a page look blurry
• A empty, or dark area appears in the center of vision
• Straight lines look distorted and out of proportionHow Is Macular Degeneration Diagnosed?
Most people are not aware that they have a macular problem until the blurred vision associated with macular problems becomes obvious. The early stages of macular degeneration can be detected during an eye examination which can include the following:• A simple Amsler grid vision test in which you are asked to look at a chart that resembles graph paper
• The macula can be viewed using an ophthalmoscope
• A fluorescein angiograph is a special photograph taken of the eye to find abnormal blood vessels under the retina. A fluorescent dye is injected via a vein in your arm and then as the dye passes through the blood vessels in the back of your eye, the photo is taken. .How Is Macular Degeneration Treated?
Despite the medical advancements of today, there is no cure for "dry" macular degeneration. Our doctors can suggest important precautions on how to protect your eyes and help slow the progression of macular degeneration. There are various new and exciting treatments that have been developed in recent years for "wet" or exudative degeneration. By the use of new laser techniques and medicines that act directly on the macula have given new hope to patients who suffer from certain forms of macular degeneration.
Migraine Syndrome
What Is Migraine Syndrome?
A migraine is a type of headache that is often hereditary and is usually first noticed between the ages of 15 and 30. Migraines are most common in women and are thought to be related to stress and even some foods.Migraine syndrome may cause some visual symptoms such as flashing lights, temporary blind spots, and blurred vision. Migraine syndrome is thought to be caused by the dilation and constriction of the arteries in the head. Migraines have been described as being extremely painful, with the pain often limited to one side of the head. Migraine headaches may be accompanied by nausea and vomiting.
Migraine headaches are often thought to be brought on by stress. Certain foods and additives can cause a migraine headache such as chocolate, alcohol, dairy, and MSG. Although the causes of migraine headaches are relatively well understood, the causes in each individual vary.
What Are The Signs & Symptoms Of Migraine Syndrome?
The symptoms of migraine headaches can vary greatly and are dependent on the underlying problem. Because the symptoms of migraine headaches is so immense, we have listed below the more common symptoms that relate to the eye.• Throbbing pain
• Increased sensitivity to light and sound
• Nausea and vomiting
• Flashing lights
• Jagged lights
• Temporary blind spots or missing areas of visionHow Is Migraine Syndrome Detected?
Your primary medical doctor should routinely obtain a complete medical history and perform a thorough physical examination to rule out systemic causes of the migraine headaches. Our doctor's will verify if the migraine headaches have any ocular involvement or not.How Is Migraine Syndrome Treated?
To help control and minimize the frequency of migraine headaches stress relief, proper control of blood pressure, or medication to maintain appropriate hormonal levels may be necessary. It may be advised that you acquire new glasses or change the lighting where you work to help minimize the frequency of migraine headaches. However, if you experience persistent migraine headaches, it is important to contact our office for an evaluation.
Ptosis

What Is Ptosis?
Ptosis is a drooping of the upper eyelid and occurs for several different reasons. Ptosis can occur as a result of disease, injury, a birth defect, having previous eye surgery and normal aging. Ptosis is often caused by weakness of the muscle that raises eyelid, also known as the levator muscle. Ptosis can also be caused by a problem with the nerve that sends messages to the muscle to contract and open. Patients who have ptosis often have difficulty blinking which may cause eye irritation and lead to infection and eyestrain.What Causes Ptosis?
Ptosis can be caused by numerous eye conditions and is usually dependent on an underlying problem. Some of these include:• Drooping lid of one or both eyes
• Eye Irritation
• Closing the eye completely is difficult
• Eye fatigue from straining to keep your eyes open
• Crossed or misaligned eye
• Double visionHow Is Ptosis Diagnosed?
When our doctor's examine a patient with a droopy lid, one of the first concerns is to determine the underlying cause of the droopy lid. Our doctor's will measure the height of the eyelid, the strength of the eyelid muscles, and evaluate eye movements and alignment. From here our doctor's will be able to determine why you have droopy lids and what the best means of treatment is.How Is Ptosis Treated?
Unlike many conditions, ptosis will not improve with time. Ptosis will almost always requires corrective surgery to fix. Usually, surgery is performed to strengthen or tighten the levator muscle and lift the eyelid. If the levator muscle is unusually weak, the lid and eyebrow may be lifted. Corrective surgery for ptosis can usually be performed with local anesthesia.
Retinal Detachment
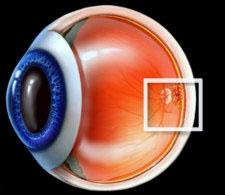
What Is A Retinal Detachment?
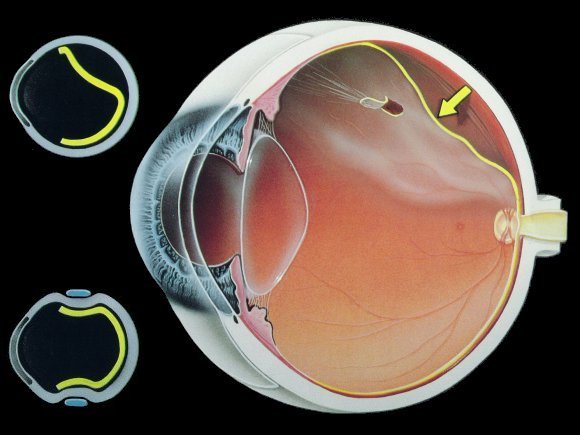
The retina is a nerve layer at the back of your eye that senses light and sends images to your brain. A retinal detachment occurs when the retina is pulled away from its normal position in the eye. The retina will not work once it is detached, causing blurred vision. Retinal detachment is a very serious problem that will almost definitely cause blindness unless it is treated promptly.What Causes A Retinal Detachment?
The middle of the eye is filled with a clear gel called the vitreous. As we age, the vitreous may pull away from its attachment to the retina at the back of the eye. Usually, the vitreous will separate from the retina without causing any problems. In some cases the vitreous pulls hard enough to tear the retina in one or more places. When this happens, it is possible for fluid to pass through the retinal tear and lift the retina off the back of the eye.
There are some conditions which may increase your chances of having a retinal detachment. Some of these include:• Nearsightedness
• Previously having cataract surgery
• Glaucoma
• Severe injury
• New onset of vitreous detachment and flashing lights
• Previously having a retinal detachment in your other eye
• Family history of having retinal detachment
• Having weak areas in your retinaWhat Are The Symptoms Of A Retinal Detachment?
There are early symptoms that may indicate the presence of a retinal detachment. These include:• Flashing lights
• Presence of new floaters
• A gray "curtain" moving across your field of visionThese symptoms do not necessarily mean that you have a retinal detachment, but it is highly recommended you contact either of our office if you are experiencing any of these. Diagnoses of retinal detachment is done during an eye examination in which your pupils are dilated, however, some retinal detachments are found during a routine eye examination.
How Is A Retinal Detachment Treated?
Most retinal tears need to be treated either with laser surgery or with cryotherapy. Cryotherapy is a term with means to freeze, or freezing. In cryotherapy the retina is sealed to the back wall of the eye. Having laser surgery or cryotherapy will cause little to no discomfort and can usually be performed in office. These methods of treatment usually prevent retinal detachment from occurring.
Most if not all patients who have a retinal detachment require surgery to put the retina back into its proper position.
What Types Of Surgery Fix A Retinal Detachment?
There are several ways in which a retinal detachment can be fixed. The type of surgery and anesthesia, either local or topical, depends on the characteristics of the retinal detachment. These methods of treatment include Pneumatic retinopexy, Scleral buckle, and Vitrectomy.
Pneumatic retinopexy - Using this method, a gas bubble is injected into the vitreous space inside the eye. The gas bubble pushes the retinal tear closed against the back will of the eye. After the procedure has been performed, you be asked to keep your head in a certain position for several days as the gas bubble gradually disappears.Scleral buckle - A flexible band known as a Scleral buckle is placed around the eye to counteract the force which is pulling the retina out of place. The fluid under the detached retina is usually drained from the eye which will allow the retina to be pulled back into its normal position against the back wall of the eye.
Vitrectomy - The vitreous gel, which is pulling on the retina, is removed from the eye and usually replaced with a gas bubble. Gradually, your bodies own fluids will replace the gas bubble. Sometimes it is necessary to combine the Vitrectomy with the use of a Scleral buckle.
What Happens After Surgery?
You can expect to have some discomfort after having surgery. You will be given necessary medications and advised when you may return to normal activity. It will be necessary after having surgery to wear an eye patch for a short period of time.
If a gas bubble was placed in your eye, it is important to follow all instructions given to you to ensure proper recovery. If you did have a gas bubble placed in your eye, it is highly suggested that you do not fly in an airplane or travel to high altitudes until the gas bubble is gone. A rapid increase in altitude can cause a dangerous rise in eye pressure.
What Are The Risks Of Surgery?
There are risks with all surgeries; however, an untreated retinal detachment usually results in permanent severe vision loss or blindness. Some of risks of having surgery to repair a detached retina include:• Infrection
• Bleeding
• High pressure in the eye
• CataractAlthough most retinal detachment surgeries are successful, it is sometimes necessary to have a second operation. If the retina cannot be reattached, then the effected eye will continue to lose sight and ultimately cause blindness.
Will My Vision Improve With Having Surgery?
It may take several months for your vision to improve, and in some cases the vision may never fully return. It is unfortunate, but some patients may not recover any vision even after having surgery. The amount of vision that will return is dependent upon the severity of the retinal detachment."Our Reputation Speaks For Itself"