Cataracts & Cataract Surgery
Questions:
- What is a Cataract?
- What Are The Symptoms Of A Cataract?
- When Should You Have Cataract Surgery?
- What Is The Cataract Surgery Procedure Like?
- What Should I Expect During Surgery?
- What Should I Expect After Having Surgery?
- What Complications May Arise During Surgery?
- What Are My Post-Operative Instructions?
- What Is In My Post-Op Kit?
What is a Cataract?
A cataract is an opacity or cloudiness in the natural lens of the eye. Cataracts are still the leading cause of blindness worldwide and represent an important cause of visual impairment in the United States. Cataracts are very common and about 1 in 7 Americans have them. About 50% of people between the ages of 65 and 74 have at least one cataract, while about 70% of people over the age of 75 have cataracts in both eyes. If we are fortunate to live long enough, we will all develop a cataract.
A Cataract develops in the lens of the eye. The normal clear lens becomes clouded, opacified and decreases the amount and quality of light entering the eye. As the cataract progresses it becomes muddy and brown and decreases a person's ability to see clearly. Just as a camera lens that has been smudged or has become dirty can spoil a photograph, the opacity in the natural lens of the eye can result in a blurred image. Patients who have cataracts often complain of blurred vision either at distance, near or both. This blurring may interfere with everyday activities such as driving or reading. Other common complaints include an increase in glare, halos, and dullness of the patient's color vision.
What Are The Symptoms Of A Cataract?
The most common symptoms include:
• Cloudy or blurry vision
• Colors seem faded
• Glare. Headlights, lamps, or sunlight may appear too bright. A halo may appear around lights
• Poor vision at night
• Double vision or multiple images in one eye
• Frequent prescription changes in your eyeglasses or contact lenses
When Should You Have Cataract Surgery?
The decision for cataract surgery is reached only between your doctor and the patient. Generally, the decision to undergo cataract surgery is based on the degree to which the patient’s vision is impaired, and the impact that impairment has on the patient's quality of life. When a patient is significantly bothered by symptoms of a cataract, cataract surgery is often recommended. Many patients will ask if a cataract must be “ripe” before surgery. With today’s technology a patient no longer must wait for the cataract to become "ripe", so the answer is “no.”
Patients will have various complaints of blurred vision, decreased color vision, problems with glare, and haze especially with bright lights and driving at night. Cataracts also impair reading vision and patients can complain of always seeing a "film" or that their glasses always seem "dirty." When cataracts impair daily function and limit your enjoyment of everyday tasks and activities, it is time to consider having cataract surgery.
Before the development of small incision cataract surgery and intraocular lens implants, the outcome of having cataract surgery was far less desirable compared to the outcomes experienced today. Therefore, ophthalmologists would typically wait until a cataract was very advanced, or "ripe", before offering surgery to the patient. Today, with advanced surgical techniques and equipment, cataract surgery can be offered at a much earlier stage. In fact, most ophthalmologists will agree that it is safer to proceed with cataract surgery at an earlier stage of development rather than waiting until the cataract is advanced and very dense. Surgery to remove the cataract and implant a clear lens is the only effective treatment to restore the priceless gift of sight.
What Is The Cataract Surgery Procedure Like?
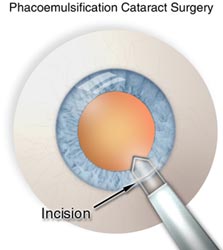
Cataract surgery today is typically performed using a microincisional procedure. Our procedure is a "No-Stitch" surgery. To the patient, this means minimal discomfort during or after surgery, less intra-operative and post-operative risks, and also a more speedy recovery of vision. We have detailed the major steps of cataract surgery using a microincision procedure, phacoemulsification (ultrasonic cataract removal), and a foldable lens implant. Cataract surgery is considered state-of-the-art by today's standards.
Below is a general overview of the basic technique. The technique used during surgery will vary based on the type of cataract, density and severity of lens change, and various associated eye conditions unique to every individual's eye.
The most commonly used cataract incision is about 3 millimeters in length– just about one-eighth of an inch! Because of the careful construction of this incision, and its extremely small size, the incision is generally self-sealing. This is the reason why this procedure is called a “no-stitch” type operation.
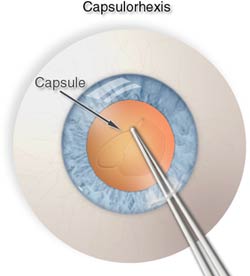
The surgeon then creates an opening in the capsule, which is a micro-thin membrane surrounding the cataract. This procedure, called capsulorhexus, requires extraordinary precision since the capsule is only about four-thousandths of a millimeter thick! This membrane is actually thinner than a red blood cell and the surgeon must delicately remove the capsule while manipulating instruments within the anterior portion of the eye. The space in the anterior chamber is quite narrow and is usually only three millimeters deep.
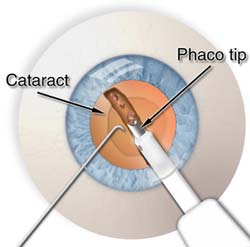
The portion of the procedure in which ultrasonic vibrations are used to break the cataract into smaller fragments is called Phacoemulsification. These fragments are then aspirated from the eye using the same instrumentation.
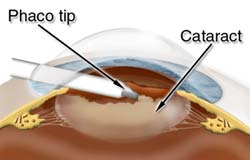
The lateral view of the procedure shows the phacoemulsification tip being placed into the substance of the cataract by the eye surgeon. The “phaco” aspect of the procedure is used to remove the denser central nucleus of the cataract.
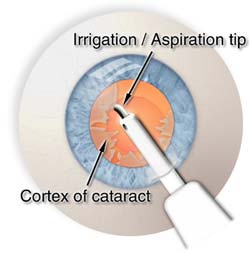
Once the denser central nucleus of the cataract has been removed, the softer peripheral cortex of the cataract is removed using an irrigation/aspiration hand piece. The posterior or back side, of the lens capsule is left intact to help support the intraocular lens (IOL) implant. We undertake meticulous polishing of this posterior capsule to ensure the sharpest and clearest vision possible.
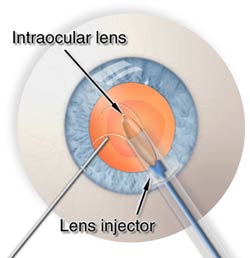

The intraocular lens is often folded and passed through the tiny incision where it is opened (implanted) inside the “capsular bag”. The lens is being inserted using an “injector”. This is an instrument designed to help keep the incision size small while allowing implantation of a 6 millimeter lens through a 3 millimeter, or possibly even smaller, incision.
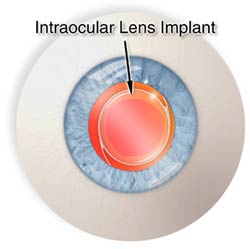

The intraocular lens (IOL) is shown implanted within the “capsular bag” where it is neatly centered. The “arms” of the IOL, known as haptics, hold the lens implant within the capsular bag.

The lateral view of the intraocular lens (IOL) implant shows the lens within the “capsular bag.” The "capsular bag" is the desired location for the intraocular lens (IOL) implant. This position is the same as that of the natural lens (cataract) of the eye and, therefore, is generally tolerated best and provides the most optimal visual results. There are special instances when the capsule cannot support an intraocular lens (IOL) implant. In these cases the lens can be placed further forward in the sulcus (space behind the iris), or the anterior chamber (space in front of the iris).
What Should I Expect During Surgery?
Modern cataract surgery is performed almost exclusively on an outpatient basis. Prior to surgery, a number of eye drop medications will be applied to the eye to prevent pain, to reduce inflammation and the risk of infection, and to fully dilate the pupil. We at Tri-State Eye perform no needle anesthesia and use topical eye drops to numb the eye.
During surgery the patient will be given mild sedation by a highly skilled anesthesiologist. The patient is asked to remain still during surgery and is kept comfortable and fully relaxed. The patient is also asked to look toward the light of the operating microscope. Cataract surgery usually takes 20 to 30 minutes to complete. Once the surgery is completed, the patient will be briefly monitored, given post-op instructions, and in most cases, the patient may be allowed to go home within an hour.
Here are a few quotes from our patients who have had cataract surgery The Tri-State Eye Way!
• "I don't know why I was nervous before the surgery-This was so easy!"
• "I didn't feel anything"
• "I haven't rested and been so relaxed in a longtime-When can you operate on my other eye?"
• "I didn't even know you started when you were telling me that the surgery was all done!"
• "This was so much easier than going to the dentist"
What Should I Expect After Having Surgery?
After discharge from the surgery center, patients will be asked to return the next day. The patient will be asked to wear a shield over the eye, particularly while sleeping. The eye should not be rubbed, or pressure placed directly on the eye through the eyelid, during the first few weeks following surgery. Eye drop medications will be required, usually consisting of antibiotic and anti-inflammatory medicines. These will often be tapered off during the first month after surgery.
The best vision may not be obtained until several weeks after having surgery, but individual results vary greatly, depending on many variables. Activities such as reading, watching television, and light work will not hurt the operated eye. We recommend waiting 4 to 6 weeks before going to get new glasses. Waiting to get new glasses allows the eye to achieve considerable stability and, therefore, the glasses prescription should be accurate.
Many patients are surprised at how clear their vision is after having cataract surgery. Some patients may have better vision than they ever did before having cataract surgery. Depending on the degree of refractive error (need for glasses) prior to surgery, many patients will be much less dependent on glasses for far vision than they ever were before having cataract surgery. Patients often notice that colors are brighter and more brilliant. The results of having cataract surgery are often dramatic.
Over 98% of cataract surgeries are successfully completed without surgical complications, and more than 95% of patients experience improved vision. Those patients whose vision fails to improve often have underlying ocular disorders, such as age related macular degeneration (ARMD), diabetic retinopathy, and other conditions. In some cases, these patients may benefit from other procedures or from low vision aids.
It is very important that you, the patient, understand that CATARACT SURGERY WILL NOT ELIMINATE THE NEED FOR, OR THE USE OF GLASSES. Even after having CATARACT SURGERY GLASSES MAY STILL BE NEEDED FOR DISTANCE & READING.
Here are some more quotes from patients that have had cataract surgery at Tri-State Eye.
• "I haven't seen this well since I've been a teenager!"
• "I can't believe how bright things are"
• "I've been walking around half-blind and didn't know it until you took off the cataracts"
• "I can't believe how bad the vision really is in my other eye-That used to be my good eye. Until I could see clearly out of the eye you operated on, I never knew how little I was truly seeing"
• "For years I've been telling people that I live in a grey house. After cataract surgery I now see that I live in a yellow house"
• "I always thought I had a clean house. After cataract surgery, I can now see all the dust"
• "I can't believe how bright and clear everything is!"
• "I can finally see clearly. I'm a safer driver because I can see again"
• "I can see where I'm hitting the golf ball again!"
What Complications May Arise During Surgery?
A complication can occur with any type of surgical procedure. Thankfully, cataract surgery performed by a skilled cataract surgeon, is one of the most successful surgeries in all of medicine and has a very low complication rate. On the rare occasion that a complication arises it can usually be treated without long-term consequences or vision loss. Complications can include, but are not limited to:
• Eyelid Drooping
• Bleeding
• Inflammation
• Infection
• Corneal Decompensation
• Damage to the Iris or other anterior segment structures
• Lens Loss
• Lens Dislocation
• Distruption of the Vitreous
• Retinal Tear or Retinal Detachment
• Retinal Bleeding
• Retinal Swelling
What Are My Post-Operative Instructions?
Resume usual pre-operative medications. Resume blood thinners. DO NOT resume eye medications that were discontinued pre-operatively unless otherwise instructed by our doctor's.
- DO NOT rub your eyes.
- Sleep on your back or your side that was not operated on for 2 weeks.
- It is permissible to bend over to put socks on and tie your shoes. You should not strain doing anything!
- You may bathe (preferred) and shower with your back to the shower. DO NOT ALLOW ANY WATER OR SOAP TO RUN OVER YOUR FACE!
- It is permissible to wash your hair as long as you do not let water or shampoo run over your face! You are allowed to go to the beauty parlor.
- The eye make take up to several months to heal after having cataract surgery.
- Try to avoid strenuous exercise for at least 2 weeks. Heavy lifting, prolonged bending over and rubbing your eyes should be avoided for 2 weeks. Walking is OK. If you are unsure of what activities you can do, please contact our offices.
If you have noticed that your eye has become: More painful, redder, has excessive discharge (pus), if you tear excessively, see flashing lights, or if your vision has worsened at any time after having cataract surgery, please contact our offices immediately.
What Is In My Post-Op Kit?
Sterile Eye Wash: Sterile eye wash for cleansing of the eye. You may need to clean or rinse the eye in the morning or during the day due to a crusting or discharge which may build up. Sterile eye pads are also included. Close the eye and squeeze some of the rinse across the eyelids. Take one of the sterile eye pads and lightly wipe the eye in a downward motion, carefully avoiding applying too much pressure.
The Plastic Eye Shield: The plastic eye shield should be used to cover your eye at bedtime, and should be worn for 2 weeks. Use two strips of tape to secure the shield in place over your eye. The plastic eye shield is to protect your eye while you are sleeping.
Dark Glasses: Dark glasses are included for protection against injury and photophobia (sensitivity to light). These glasses can be worn inside as well as outside if needed. These glasses will fit over your regular glasses if you choose to wear them this way. It is important to wear a pair of glasses at all times to protect the eye, especially the first couple of weeks after having surgery.
"Our Reputation Speaks For Itself"